Q&A: Health care exchanges
People nationwide began signing up Oct. 1 for health insurance coverage under the federal Affordable Care Act through online marketplaces called exchanges.
States had the option of setting up their own exchange or allowing the federal government to do it. In North Carolina, the federal government set up a system so individuals and small-business owners can compare the costs and coverage offered by various insurers.
Blue Cross Blue Shield of North Carolina and Coventry Health Care of the Carolinas are offering dozens of plans through the exchange. FirstCarolinaCare withdrew its plans to participate, citing uncertainties with the exchange's operation.
Coverage through the exchange-based health plans starts Jan. 1, 2014, when the Affordable Care Act's requirement for people to have insurance kicks in. Most people who forgo insurance coverage will face a tax penalty. The government delayed until 2015 a similar mandate for companies with at least 50 employees to provide affordable health coverage to their workers or face penalties.
Although open enrollment for coverage through the exchange ends March 31, people wishing to have coverage on Jan. 1 must enroll by Dec. 15.
Q: Who should consider buying insurance through an exchange?
A: Whether you’re uninsured, you’ve been denied coverage in the past or you just want to explore new options, the exchange can provide you some choice and control over your health coverage.
The exchange simplifies the search for coverage by gathering the options available in each state in one place. You can compare plans based on price, benefits, quality and other features important to you before making a choice. Then, with one application, you can see all available insurance options and enroll.
By law, information about prices and benefits must be written in simple language, so you get a clear picture of what premiums you will pay and what benefits and protections you will get before you enroll. You can compare plans based on what's important to you and choose the combination of price and coverage that fits your needs and budget.
Q: What does an exchange health plan cover?
A: All plans offered through the exchange will meet minimum coverage requirements, including the following benefits:
- Outpatient care
- Emergency services
- Hospitalization
- Maternity and newborn care
- Mental health and substance use disorder services, including behavioral health treatment
- Prescription drugs
- Rehabilitative services and devices
- Laboratory services
- Preventive and wellness services and chronic disease management
- Pediatric services
Unless they are sponsored by certain exempt religious employers, plans also must cover birth control methods, including so-called day-after pills, and counseling. They are not required to cover drug-induced or surgical abortions.
Some plans may offer additional coverage beyond the minimum requirements.
Q: How do I choose a plan on the exchange?
A: The exchange divides its health plans into four categories: Bronze, Silver, Gold and Platinum. The category you choose affects how much your monthly premium costs, what portion of the bill you pay for things like hospital visits or prescription medications and your total out-of-pocket costs.
With a Bronze plan, you'll likely pay a lower premium but will pay a higher share of costs – through co-payments and deductibles – when you get care. Platinum plans will likely have the highest monthly premiums and lowest out-of-pocket costs.
Q: How much does each plan cost?
A: Costs and coverage are spelled out on the exchange website.
Q: What's the difference between exchange plans and other health coverage?
A: Starting in 2014, all health insurance plans must offer at least the benefits listed above. You can purchase the same coverage offered through the exchange directly from Blue Cross or Coventry or through an independent insurance agent, but if you qualify for a federal subsidy to lower the cost of your monthly premiums, you must enroll through the exchange to obtain that subsidy.
The lower costs are handled through a tax credit, which can be applied directly to your monthly premiums.
The amount you save depends on your family size and annual income. In general, if your income falls within the following ranges, you will qualify for lower premiums in 2014:
- $11,490 to $45,960 for individuals
- $15,510 to $62,040 for a family of 2
- $19,530 to $78,120 for a family of 3
- $23,550 to $94,200 for a family of 4
- $27,570 to $110,280 for a family of 5
- $31,590 to $126,360 for a family of 6
- $35,610 to $142,440 for a family of 7
- $39,630 to $158,520 for a family of 8
Families that fall below the ranges likely qualify for Medicaid coverage.
If you qualify for out-of-pocket savings, you must choose a Silver plan to get the savings. You can still choose any category of plan, but will get the out-of-pocket benefits of a Gold or Platinum plan for a cheaper price only if you enroll in a Silver plan.
Q: Can I keep my current doctors?
A: Depending on the plan you choose in the exchange, you may be able to keep your current doctor. Most of the plans have networks of hospitals, doctors, specialists, pharmacies and other health care providers. Depending on the type of policy you buy, care may be covered only when you get it from a network provider.
When comparing exchange plans, you should check each plan's network if staying with your current doctors is important to you.
Q: What if I have health insurance through my job?
A: If you have job-based insurance that you like, you can keep it. You're considered covered under the Affordable Care Act.
If you want to switch to coverage through the exchange, you may, but you need to consider a couple of caveats:
Most employers pay a portion of the premiums for their workers, but anyone choosing an exchange plan likely wouldn't get a subsidy for premiums from their employer. Also, if your job-based insurance is considered affordable and meets minimum value, you cannot get any lower premiums or out-of-pocket expenses through an exchange plan, even if your income meets federal guidelines.
Q: What if I own a business?
A: The Affordable Care Act permits small businesses that wish to keep the insurance plan they currently have to do so. So-called "grandfathered" group plans are subject to fewer requirements under the law, such as not having to meet the minimum coverage outlined above.
If a company’s plan was in place before March 23, 2010, and is grandfathered, the company can add new members and even change insurers as long as the benefits and costs to employees stay largely the same. If benefits are cut or employees are asked to shoulder a larger percentage of the costs, the plan loses its grandfather status, and the company must adopt a new plan through the Small Business Health Options Program (SHOP) if it wishes to continue providing health coverage to workers.
SHOP is open to employers with 50 or fewer full-time-equivalent employees. The threshold will increase to 100 employees in 2016.
SHOP allows employers to control the coverage they offer and how much they pay toward employee premiums. They also might qualify for a small-business health care tax credit worth up to 50 percent of their premium costs. (The remainder of the premium costs can be deducted on a federal income tax return.)
To participate in SHOP, a business owner must offer coverage to all full-time employees. In many states, at least 70 percent of the employees must enroll in plan.
Like grandfathered plans, businesses with self-funded health coverage – those where the employer accepts the risk for the health benefits it provides rather than buying coverage from an insurance company – don't have to meet the minimum coverage under the Affordable Care Act. They must, however, extend dependent coverage until age 26, provide preventive services with no co-payments and include no annual or lifetime limits on coverage.
Q: What if I'm self-employed?
A: If you own a business where you are the only employee or you use only independent contractors to help with the work, you can apply for coverage through the general exchange and not through SHOP.
Q: What if I have a pre-existing condition?
A: Being sick won't keep you from getting health coverage. An insurance company cannot turn you down or charge you more because of your condition.
Once you have insurance, it can't refuse to cover treatment for pre-existing conditions. Coverage for such conditions begins immediately, even if you have been turned down or refused coverage before.
The only exception is for grandfathered individual health insurance plans – the kind you buy yourself, not through an employer. They do not have to cover pre-existing conditions.
If you have one of these plans, you can switch to an exchange plan during open enrollment and immediately get coverage for a pre-existing condition.
Q: What if I have Medicare?
If you have Medicare, you are considered covered under the Affordable Care Act, and you don't need to enroll through the exchanges.
Medicare benefits now include the minimum benefits outlined above that are required of health plans offered through the exchanges.
Medicare has its own enrollment period, which runs through Dec. 7. Anyone who is close to turning 65 needs to enroll either through Medicare.gov or at a Social Security office, even if you are still working.
Q: Can I buy catastrophic health coverage?
A: People under 30 and older individuals with limited incomes may buy a catastrophic plan that requires them to pay all medical costs up to a certain amount, usually several thousand dollars.
Catastrophic policies offered through the exchange cover preventive care and three primary care visits per year at no cost. People who purchase such plans cannot get tax credits for monthly premiums or on lower out-of-pocket costs based on their income.
Q: What if I need coverage before January 2014?
A: If you don’t have coverage now and need it before January, you can buy directly from an insurance company.
Be aware that some protections and benefits of the Affordable Care Act aren't yet in effect and may not apply to your coverage, such as denial of coverage for a pre-existing condition and a lack of subsidy to assist with the premiums.
Also, you may want to find out when you can stop your policy – at any time or only at the end of a plan or policy year.
Q: What happens if I don't have health insurance?
A: The Affordable Care Act requires all people who can afford it to take responsibility for their own health insurance by getting coverage or paying a penalty. People without health coverage will also have to pay the entire cost of all their medical care.
The fee in 2014 is 1 percent of annual income or $95 per person, whichever is higher, and the fee will increase every year. The fee for uninsured children is $47.50 per child in 2014.
The only people living in the U.S. who can avoid the fee without health coverage are those who are uninsured for less than three months of the year, have very low incomes and cannot afford coverage, would qualify for Medicaid under new income guidelines but live in North Carolina or another state that hasn't expanded Medicaid eligibility, are a member of a federally recognized Indian tribe, are in prison, are an undocumented immigrant, participate in a health care sharing ministry or are a member of a recognized religious sect that objects to health insurance.
Health insurance plans will provide documents to people they insure to prove that they have the minimum coverage required by law, and the IRS is developing rules for including such information on federal income tax returns. The fees assessed for not having coverage will be collected through tax returns.
Q: Where I can find more information or get help with enrollment?
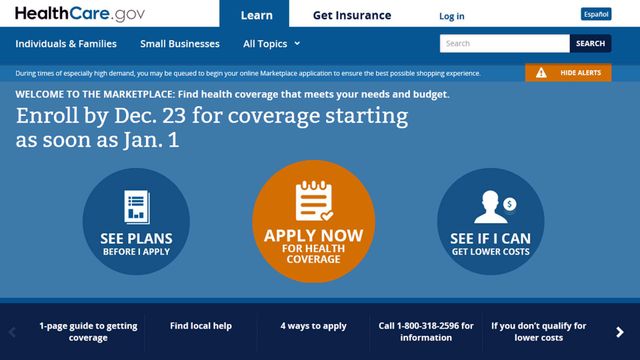
A: Visit HealthCare.gov or call toll-free 800-318-2596
Q: Are the delays and technical glitches resolved on the Affordable Care Act website?
A: Three weeks after its launch, the federal website to explore and compare benefits continued to show delays.
Federal officials said they are working to improve the website amid continued high traffic, adding server capacity and making hardware and software adjustments. They also recommended that people call the above-mentioned help line to enroll over the phone or to seek out local "navigators," who are trained to provide assistance with enrollment. The HealthCare.gov site provides city-by-city lists of navigators working nationwide.