Once hospitalized for tick-borne allergy, Raleigh man learns he can eat meat again
When Scott got to the emergency department that night in September 2018, medical staff took him right in.
"They said I was pretty close to anaphylactic shock,” Scott said, describing the allergic reaction.
It was by far the worst in a series of reactions over the previous weeks.
“I was having a hard time...talking,” Scott said. “My eyes were puffy; I could hardly see. It was scary.”
The cause was a tick bite that left him allergic to meat.
Scott lives in Raleigh. He talked with 5 On Your Side's Monica Laliberte about his struggles with hives and, at times, swelling before a blood test finally revealed he suffered from alpha-gal syndrome.
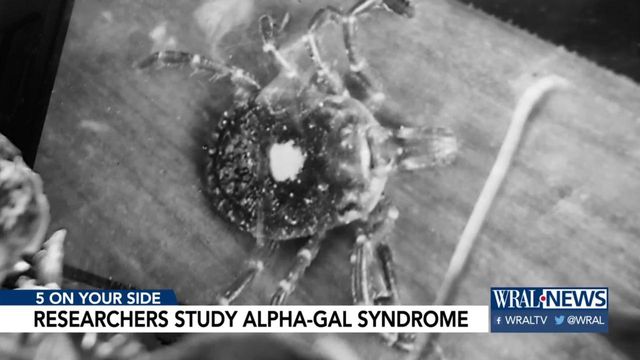
It's named after a sugar molecule transmitted to humans by Lone Star ticks.
Female ticks are known for a blotch of white on their backs.
Alpha-gal syndrome is one of potentially 10 different complications that can follow a tick bite.
Lyme is one of the most commonly known. Encephalitis is another. Sen. Kay Hagan had it for three years before dying in October.
Alpha-gal syndrome leaves patients severely allergic to the meat of mammals: beef, pork, lamb, venison, buffalo and bison.
It was so severe for Scott that he had to start carrying an Epipen.
Early research shows alpha-gal syndrome is spreading across the United States.
The CDC says most cases are in the Southeast and Midwest.
A world map of self-reported cases reflects that.
Many cases are pinned in North Carolina, especially in the central part of the state.
"This tick is expanding in its geography and its numbers," said Dr. Scott Commins, a leading alpha-gal researcher with UNC School of Medicine's Division of Rheumatology, Allergy and Immunology.
He says the syndrome is difficult to diagnose for a couple reasons.
First, it can take weeks to establish itself in a person.
Then symptoms, from swelling and a rash to severe stomach pain, can take hours to show after eating meat.
https://www.mayoclinic.org/diseases-conditions/alpha-gal-syndrome/symptoms-causes/syc-20428608
Many patients react to anything associated with mammal ingredients: milk, cheese, cosmetics, medicines.
"Even like a capsule, a gelatin capsule," Commins said. "The gelatin often comes from the hooves of horses, and that would contain alpha-gal."
For some, just the steam from bacon or wool in clothes can trigger a reaction.
But not everyone bitten by a Lone Star tick gets alpha-gal syndrome, and researchers are trying to figure out why that is.
One common trend in diagnosed cases is a specific reaction to the tick bite.
“Often, patients will say ‘You know, I've been bitten for years, but one of my bites turned large and red and itchy and swollen and it persisted for months ... and it was quite slow to heal,’” Commins shared. “That's often the index bite that seems to trigger this response."
Commins said they are actively looking into what suddenly makes a bite an index bite.
The reaction is what Scott experienced after his bite. It happened while doing some clean-up in his backyard.
But a year after his medical emergency, Scott got some shocking news.
After avoiding meat, a follow-up blood test revealed his alpha-gal syndrome was gone.
"My alpha-gal panel was negative," he said. "When the nurse called me, I said `What exactly does that mean because that, that doesn't even seem like it's possible.'"
But is was possible: He no longer showed signs of the meat allergy.
"We think this goes away over time, so we need to follow patients for several years to see," Commins said. "It seems like it almost wants to go away."
"I don't think we can stop it from starting," he said. "But if we can prevent those additional bites from perpetuating it, then you're off meat for two, three, four years."
It's another area researchers are looking into.
With no signs of the allergy, Scott got the green light to re-introduce mammal meat to his diet.
He started with a quarter slice of bacon, then a half slice, then, by the end of the week, a full slice.
He did it with no reaction.
While relieved, he still carries an Epipen just in case.
"I don't want to end up where I was a year ago," Scott said. "It was scary."
If any patients want to be part of any current studies, they can call (919) 966-2059 to get involved. The line is not staffed constantly, so you’re encouraged to leave a message.