New data shows cancer deaths on decline, new diagnoses hit record high
The latest annual report by the American Cancer Society (ACS) shows cancer mortality is on the decline but projected new diagnoses are expected to set a new record.
For the first time, new cancer diagnoses are projected to top 2 million, according to the report released Wednesday. That is an average of 5,480 new diagnoses each day.
Dr. Bill Dahut, chief scientific officer at ACS, said the increase could partly be attributed to advancements in detection technology. However, he specified the reason the report is cause for alarm is because most of the cancers that saw increases in diagnoses were those that aren’t routinely screened for, such as liver and pancreas cancers.
Rise of colon cancer in younger adults
The rise in colorectal cancer diagnoses in adults younger than 50 is also causing concern. Over the past 20 years, colorectal cancer has grown from being the fourth leading cause of death in younger men and women to the first in men and second in women behind breast cancer.
Dr. Ahmedin Jemal, senior vice president at ACS, said increasing screenings and promoting awareness of non-invasive stool tests could help reverse the trend, specifically in those ages 45 to 49 years old.
“We really need to understand why rates are increasing in those age groups and at the same time plan intervention,” Jemal said.
The American Cancer Society recommends those at average risk start colon cancer screenings at 45 years old. Those with a known family history of cancer should begin screenings earlier, Dahut said.
“A clinical rule of thumb is, in general, one should consider screening for a cancer 10 years prior to a cancer diagnosis in your immediate family,” he said. “30% of new colorectal diagnoses for people under the age of 50 were for those not at average risk.”
Cervical cancer increases in middle-aged women
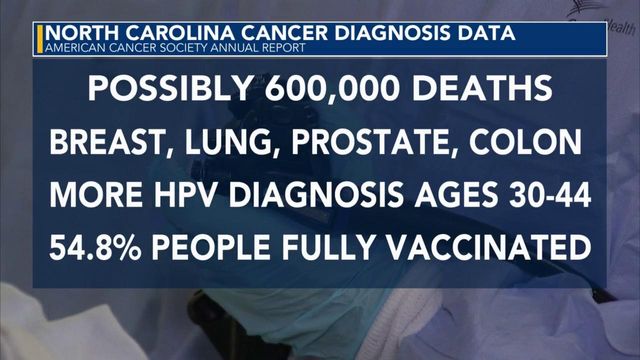
The report shows cervical cancer has gone down in women in their 20s but increased nearly 2% among those 30 to 44 years old. The change highlights the importance of receiving the HPV vaccine and increasing screenings in young women.
According to Americas Health Rankings, 54.8% of North Carolinians between the ages of 13 to 17 had received all doses of the HPV vaccine in 2022. That is a decline of 13% compared to the year prior. North Carolina now ranks among the worst states in the country for HPV vaccinations, at sixth-lowest overall.
Cancer in teens and younger children
Cancer in teens ages 15 to 19 years old continues to increase, while incidences of cancer in younger children seem to be leveling off, according to the new study. The ACS reports the largest increase was a 4% rise in thyroid cancer, which is sourced to “likely overdiagnosis.”
While mortality rates overall are on the decline, endometrial cancer deaths saw a slight 2% increase. Black women are at a specific risk (9.1 per 100,000) for endometrial cancer deaths compared to white women (4.6 per 100,000).
People of color more likely to die from cancer
Disparities are also prevalent among prostate, stomach and uterine cancers with Black individuals twice as likely to die. Native American individuals are also at twice as high risk of death for liver, stomach and kidney cancers.
“Often times, a great proportion of a difference of outcomes is driven by access to equitable care,” said Dahut. “I think we need to ensure people not only have access to care, but access to equitable care.”
The new study also showed diagnoses across the board are happening earlier in life than before. There was a 5% increase in diagnoses among middle aged adults (50 to 64 years old) from 25% in 1995 to 30% between 2019 and 2020. Comparatively, diagnoses among those 65+ decreased by 3% from 61% to 58%.
Cancer and the pandemic
This year’s study also marked the first time data from the pandemic was included.
“We see there’s a 9 to 10% drop in the incidence rate in 2020 versus 2019. This is because of healthcare closures related to the pandemic and largely because of less screenings. We knew that was happening at the time,” said Rebecca Siegel, senior scientific director with ACS surveillance research.
Siegel explained a lack of routine screenings and imaging led to a lower diagnoses rate during the pandemic because early-stage diseases weren’t being caught. She continued to state it will still take more time for advance diseases that were missed to be diagnosed and said “this will happen gradually.”
"What will take even more time is to see the impact on mortality,” said Siegel. “It’s possible that this will trickle in so gradual overtime that we may not even see an impact on mortality that we can say for certain is related to COVID. It’s really just a wait and see, but right now we do see this big drop in incidence rate in 2020.”
Seigel said there is some indication the incidence rate will go up again when 2021 data is available.
Cancer screening is critical
To reduce the prevalence of cancer in society moving forward, Dahut said more people need to be screened for cancers for which early testing is available, such as lung cancer.
“Lung cancer screening uptake among those who are eligible remains abysmal. In many parts of the country it’s under 10%,” he said.
He also emphasized the need for more resources to be devoted to developing improved therapies for cancers like liver and pancreatic cancers along with rare sarcomas, that don’t have good screening methods.
Dahut also said there are small changes people can make in their everyday lives that could have major health benefits in the long-run.
“About 42% of cancers in this country are preventable, which is an incredibly high number. Perhaps half of that is tobacco. If people can really eliminate tobacco use at any age, specifically as a young adult and if you can really stop smoking before you’re 30, the impact is really significant,” he said.
Dahut continued, “Get your HPV vaccination. It has been targeted at women and boys as adolescents and early adults, but there is increasing evidence that if you don’t have an HPV vaccination, you should continue to consider that vaccination once you’re beyond that age.”
The doctor also emphasized the importance of exercise saying, “Exercise alone will save lives, regardless of other factors like obesity. Even getting out of your chair and walking around the room for five minutes every hour is hugely important.”