NC investigating 206 providers for potential Medicaid fraud
One day after the WRAL Investigates team reported on potential fraud in North Carolina's Medicaid system, the state Department of Health and Human Services announced that it is investigating 206 providers across the state with unusual Medicaid billing.
Posted — UpdatedMost of the potential fraud cases are local, with 103 in the Triangle, 43 in the Charlotte area and 24 in Greenville and surrounding counties, state officials said. Ten of those cases have been turned over the state Attorney General's Office for review.
The WRAL Investigates team reported Monday that 23,000 billing hours were linked to a licensed therapist in Wake County last year, even though there are only 8,760 hours in a year.
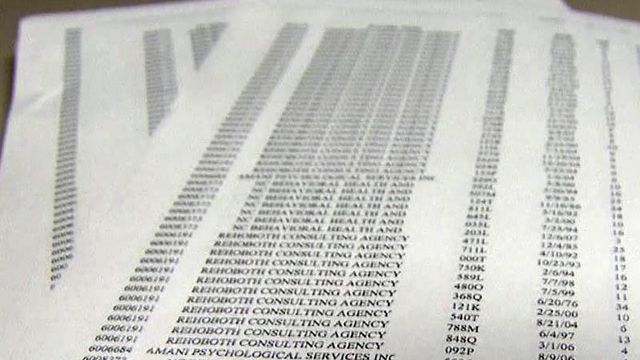
Billing records show psychologist Eunice Ngumba-Gatabaki worked, on average, 60 hours per day, which cost the state $1.79 million last year.
"People should be outraged," said Gov. Bev Perdue. "Those are dollars that aren't there to treat older sick people or children."
Gatabaki's daily average increased last June as records show she worked more than 100 hours per day for 17 days. She says "there may have been some bills inadvertently billed under my provider number that may be attributable to other licensed providers."
Through her attorney, Gatabaki admits she signed off on other therapists' work but says Raleigh-based Rehoboth Consulting did the actual billing.
Gatabaki’s name was also linked to more than $676,000 in Medicaid billing through N.C. Behavioral Health and Counseling. She denies any link to the agency.
"It's outrageous," said Rep. Nelson Dollar, R-Wake, who chairs the DHHS oversight committee. "It does make you angry ... We need to make sure not one dime of taxpayer money is being wasted."
Last year, North Carolina spent about $10 billion on taxpayer-funded Medicaid claims, covering everything from doctors’ bills to mental health care for low-income residents. With help from IBM, the state has a new tool to crack down on fraudulent claims, which experts say could make up as much as 2 percent or $200 million each year.
The new fraud detection computer program from IBM uses math and statistics to find abnormalities in Medicaid claims. North Carolina is the first and only state in the country using it.
IBM anti-fraud solutions leader Shaun Barry says the tool helps point investigators in the right direction. “It tells them where to look … what rocks to look under, if you will,” he said.
"The department needs to accelerate their efforts," Dollar said. "I think the IBM solution on this needs to start showing some real results."
• Credits
Copyright 2024 by Capitol Broadcasting Company. All rights reserved. This material may not be published, broadcast, rewritten or redistributed.