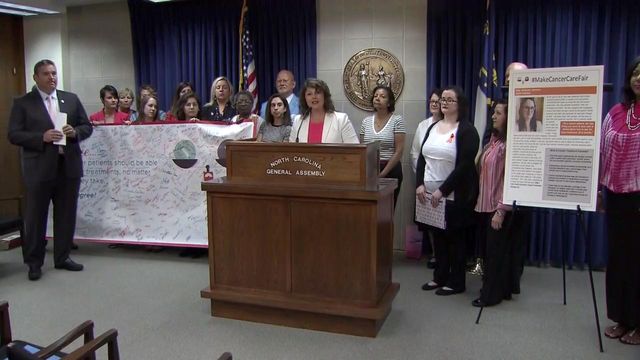
Advocates call for fairness in chemo coverage
Cancer patients and advocates on Wednesday called on the state Senate to pass legislation requiring insurers to cover oral chemotherapy drugs in the same way that they cover injected or IV-administered chemotherapy protocols.
Posted — UpdatedThe House has passed such legislation in each of the past three sessions, but bills have repeatedly stalled in the Senate.
Under current law, health insurance companies charge a flat co-pay per procedure for chemotherapy that's administered via IV or injected. Many newer therapies are oral drugs – a pill the patient takes, rather than a procedure – and insurers classify that as a prescription drug and require a higher co-pay.
Amy Riggleman said she has to pay $200 a month for generic medication to treat her leukemia, and the cost would be much higher if she didn't receive financial assistance arranged through UNC Hospitals.
"I work two jobs to afford to battle cancer," the 27-year-old Garner woman said. "No one who pays for health insurance should have to potentially forgo cancer treatment that they need because insurers don't want to cover anti-cancer oral chemotherapies in a fair way. It is time to make cancer care fair in North Carolina."
"Patients do not choose what kind of cancer they get. They should not have to choose whether or not they will treat it simply because of the type of health insurance coverage they have," Lewis said. "All we're seeking here is parity. We're not trying to seek any special treatment for oral cancer drugs."
Blue Cross Blue Shield of North Carolina, the state's largest health insurer, said the cost of oral chemotherapy has soared by 500 percent since 2000, and capping the portion that patients pay would force premiums up across the board. If the legislation is approved, Blue Cross said, it would eliminate the incentive for drug companies to negotiate lower prices with insurers and would allow them to continue raising prices, which would continue driving up premiums.
Mary Catherine Moffett, director of advocacy for the Leukemia & Lymphoma Society, said other states that have adopted similar chemotherapy parity laws have seen negligible increases in insurance premiums.
"If a cancer patient's treatment is covered in their plan, it should be covered in the same way regardless of how it is administered," Moffett said.
Related Topics
• Credits
Copyright 2024 by Capitol Broadcasting Company. All rights reserved. This material may not be published, broadcast, rewritten or redistributed.